Diverticular surgery in Iran
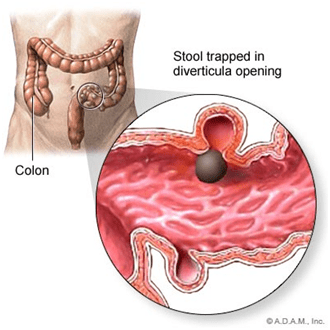
Diverticular surgery in Iran is a procedure performed to treat complications arising from diverticulosis, which is a condition where small, bulging pouches (diverticula) develop in the digestive tract, most commonly in the colon.
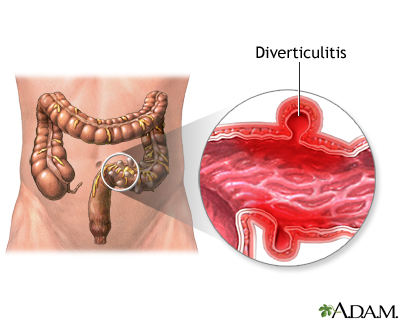
When these pouches become inflamed or infected—a condition known as diverticulitis—surgery may be necessary if the condition is severe, does not respond to medical treatment, or if complications occur.
Types of Diverticular Surgery in Iran
There are two main types of surgery for diverticulitis:
1. Primary Bowel Resection
– The surgeon removes the diseased part of the intestine and then reconnects the healthy segments (anastomosis). This can often be done with a minimally invasive approach (laparoscopically) depending on the extent of the disease and if there is no significant inflammation or other complications.
2. Bowel Resection with Colostomy
– If the inflammation is severe or there’s an infection outside the colon, the surgeon may not be able to rejoin the colon and rectum. In this case, a colostomy is performed. A colostomy involves creating an opening in the abdominal wall (stoma) for the removal of waste, which collects in a bag outside the body. The colostomy may be temporary, especially if the colon needs time to heal, or it can be permanent if a large portion of the colon is removed.
Indications for Surgery
Surgery for diverticulitis is typically recommended for:
- – Recurrent episodes of diverticulitis that cause severe symptoms or complications
- – A significant or life-threatening complication like perforation, abscess, fistula, or bowel obstruction
- – Immunosuppressed patients with an episode of diverticulitis due to an increased risk of complications
- – Patients who do not respond to conservative treatment with antibiotics and diet changes
- – Certain cases of complicated diverticulitis with either a large abscess or a phlegmon (inflamed area of tissue)
Risks and Considerations
Like all surgeries, diverticular surgery comes with risks, which may include:
- – Bleeding
- – Infection
- – Adverse reactions to anesthesia
- – Injury to nearby organs
- – Blood clots
- – Incisional hernia
- – Complications from a colostomy if one is performed
Recovery
Recovery from diverticular surgery in Iran varies depending on the individual patient, the type of surgery, and whether there were any complications. For minimally invasive procedures, recovery may be quicker, with many patients returning to normal activities within a few weeks. Open surgeries or those with complications may require a longer recovery period.
During recovery, patients may need to adhere to a specific diet, avoid heavy lifting, and attend follow-up appointments to ensure proper healing. If a colostomy is performed, patients will also need education on colostomy care and management.
Conclusion
Diverticular surgery in Iran is a major procedure and is typically reserved for those with serious or recurring issues related to diverticulitis. Decisions regarding surgery should be made in consultation with a gastroenterologist and a colorectal surgeon, taking into account the individual’s health status, risks, and potential benefits.
What to expect from Diverticular surgery in Iran
If you’re preparing for diverticular surgery, it’s important to know what to expect before, during, and after the procedure. Here’s a general overview:
Before Surgery
- – Preoperative Evaluation: You’ll undergo a thorough evaluation, which may include blood tests, imaging studies, and a colonoscopy to assess the extent of the diverticular disease.
- – Bowel Prep: You may be asked to follow a clear liquid diet and take a bowel prep to cleanse the colon before surgery.
- – Fasting: Typically, you’ll be instructed to refrain from eating or drinking anything after midnight on the day before your surgery.
- – Medication Adjustments: Your doctor may adjust your medications, especially if you’re on blood thinners or have diabetes.
- – Consent: You’ll discuss the risks, benefits, and potential complications of the surgery with your surgeon and give informed consent.
During Surgery
- – Anesthesia: You will be given general anesthesia, so you will be asleep and pain-free during the procedure.
- – Incision: Depending on whether the surgery is open or laparoscopic, the surgeon will make a large incision or several small incisions.
- – Resection: The surgeon removes the affected portion of your colon.
- – Reconstruction: The healthy parts of the colon are then reconnected, or a colostomy is performed if necessary.
- – Duration: Surgery can last several hours, depending on the complexity and whether additional procedures are required.
After Surgery
- – Recovery Room: Immediately after surgery, you’ll be taken to a recovery room where your vital signs are monitored as you wake up from anesthesia.
- – Hospital Stay: The length of the hospital stay can vary from a few days to a week or more, depending on the type of surgery and your individual recovery.
- – Pain Management: You will receive pain medication to manage any discomfort post-surgery.
- – Diet: Your diet will gradually progress from clear liquids to more solid foods as your bowel function returns.
- – Activity: You’ll be encouraged to move around as soon as possible to help prevent blood clots and pneumonia, and to promote healing.
- – Wound Care: If you have an open incision, you’ll be taught how to care for it to prevent infection.
- – Colostomy Care: If you have a colostomy, a stoma nurse will teach you how to care for it.
- – Monitoring: Your healthcare team will monitor for any signs of complications, such as infection or bleeding.
Recovery at Home
- – Activity Restrictions: You’ll need to avoid heavy lifting and strenuous activities for several weeks.
- – Follow-Up Appointments: You’ll have follow-up appointments to monitor your recovery and to remove any stitches or staples.
- – Medication: You may continue to take pain medication and other prescriptions as directed by your doctor.
- – Diet: You might need to follow a specific diet to ease your digestive system back into normal function.
- – Symptom Monitoring: You should monitor for symptoms of complications, such as fever, severe abdominal pain, or unusual discharge from the incision site.
Long-Term Expectations
- – Dietary Adjustments: You may need to make permanent changes to your diet, such as increasing fiber intake to promote regular bowel movements and prevent future diverticular disease.
- – Lifestyle Changes: Maintaining a healthy weight, exercising regularly, and not smoking can help prevent further issues.
- – Regular Checkups: Ongoing medical follow-ups may be necessary to monitor your digestive health.
It’s important to closely follow your surgeon’s instructions throughout the entire process. Open communication with your healthcare team about any concerns or symptoms you experience during recovery is crucial. Each patient’s experience is unique, and recovery can vary widely from person to person.
Recovery after Diverticular surgery
Recovery after diverticular surgery varies based on the individual’s health, the type of surgery performed (laparoscopic or open), and whether there were any complications during or after the surgery. Here’s an outline of what recovery typically involves:
Immediate Postoperative Period
- – Hospital Stay: After surgery, you will typically stay in the hospital for a few days to a week or more. Laparoscopic surgery often has a shorter hospital stay compared to open surgery.
- – Pain Management: You’ll receive pain medication to manage post-surgical discomfort. Initially, this may be administered through an IV and later switched to oral medication.
- – Monitoring: Medical staff will monitor you for signs of complications, such as infection, bleeding, or issues with the anastomosis (the join where the bowel has been reconnected).
- – Catheters and Drains: You may have a urinary catheter placed during surgery, which is usually removed within a day or two. If drains were placed in your abdomen to remove excess fluid, they’ll be monitored and removed when appropriate.
Early Recovery at Home
- – Activity: Gradually increase your activity level as recommended by your doctor. Walking is encouraged to help prevent blood clots and improve bowel function.
- – Incision Care: You will be instructed on how to care for your surgical incision and what signs of infection to watch for.
- – Diet: You’ll likely start with clear liquids and gradually progress to solid foods as bowel function returns. High-fiber foods may be recommended to help prevent future episodes of diverticulitis.
- – Hydration: It’s important to stay well-hydrated to help the bowel function properly and to aid in overall recovery.
- – Medication: Take any prescribed medications, including antibiotics or pain relievers, as directed.
- – Follow-Up Appointments: Keep appointments with your healthcare provider to check your recovery progress and to address any concerns.
Ongoing Recovery
- – Activity Restrictions: Avoid heavy lifting and strenuous activities for several weeks, according to your doctor’s advice.
- – Colostomy Care: If you have a colostomy, you’ll need ongoing education and support to manage it effectively.
- – Symptom Monitoring: Stay alert for symptoms such as fever, worsening pain, redness or discharge from the incision, or changes in bowel habits, and report these to your doctor.
- – Dietary Changes: Gradually reintroduce different foods into your diet. Some individuals may need to avoid seeds, nuts, and popcorn, though recent evidence suggests they may not be as problematic as once thought. Your healthcare provider will give you guidance based on the latest research and your specific condition.
- – Physical Therapy: Some patients may benefit from physical therapy to strengthen abdominal muscles, especially after an open surgery.
Long-Term Recovery
- – Lifestyle Changes: Adopting a healthier lifestyle is key to reducing the risk of future diverticular complications. This includes regular exercise, a balanced high-fiber diet, staying hydrated, and avoiding smoking.
- – Regular Checkups: Continue with regular medical checkups to monitor your overall health and digestive system.
- – Possible Reversal of Colostomy: If the colostomy was temporary, another surgery might be scheduled to reverse it once healing is complete and the inflammation has resolved.
Emotional and Psychological Support
– Support Groups: Consider joining a support group for individuals who have undergone similar surgeries to share experiences and coping strategies.
– Mental Health: Be mindful of your mental health. It’s not uncommon to experience feelings of anxiety or depression after major surgery, and professional support can be beneficial.
Recovery can be a complex process, and it’s important to give your body the time it needs to heal. Always communicate with your healthcare team and follow their instructions carefully. They will provide guidance tailored to your specific situation. Remember, while general information can be helpful, personalized medical advice from your healthcare provider is invaluable for a safe and effective recovery.
Diet after Diverticular surgery
After diverticular surgery, dietary adjustments are an important part of the recovery process. The goal is to allow your digestive system to heal and gradually return to normal function while preventing future episodes of diverticulitis. Here is a general guideline on the diet after diverticular surgery, but make sure to follow the specific advice provided by your healthcare team as individual recommendations may vary.
Immediate Post-Surgery Diet
1. NPO (Nil Per Os): Immediately after surgery, you may not be allowed to eat or drink (this is commonly referred to as NPO, which is Latin for “nothing by mouth”) until bowel function begins to return. This is to ensure that the bowel can heal without being stressed by the digestion process.
2. Clear Liquid Diet: Once you are cleared to eat and drink, you will typically start with a clear liquid diet. This includes foods that are clear and liquids at room temperature, such as:
– Water
– Clear broths
– Apple juice
– Ice chips
– Gelatin (without added fruits or toppings)
– Popsicles
3. Full Liquid Diet: If you tolerate clear liquids, you may then progress to a full liquid diet, which includes:
– Milk and milk products
– Strained creamy soups
– Vegetable juice
– Fruit juices without pulp
– Cooked, refined cereals like cream of wheat
Transition to Solid Foods
1. Low-Fiber Diet: Once you can tolerate liquids, you might be advised to eat low-fiber foods, which are easier on your digestive system as you continue to heal. Low-fiber foods include:
– White bread, pasta, and rice
– Well-cooked vegetables without skin or seeds
– Eggs
– Dairy products (if not lactose-intolerant)
– Lean meat, fish, and poultry
2. Soft Diet: As your bowel continues to heal, you can gradually start to add soft foods that are easy to chew and swallow, such as:
– Cooked fruits and vegetables
– Canned or soft fresh fruits without seeds or skin
– Low-fiber cereals
– Tender meats
Progression to High-Fiber Diet
1. High-Fiber Foods: Once your doctor feels you are ready, usually after a few weeks, you’ll be encouraged to start incorporating high-fiber foods into your diet to help prevent constipation and further diverticular issues. These include:
– Whole grains (like whole wheat bread, brown rice, quinoa, and oatmeal)
– Fresh fruits and vegetables
– Beans and legumes
– Nuts and seeds (some doctors may still recommend avoiding these, so follow your doctor’s advice)
2. Fiber Intake: The recommended amount of fiber is generally 25 to 30 grams per day. Increase fiber intake slowly to prevent gas and bloating.
Important Considerations
- – Hydration: Ensure adequate fluid intake, especially when increasing fiber in the diet, to help maintain bowel regularity.
- – Chew Well: Chew food thoroughly to aid in digestion and reduce the workload on your digestive tract.
- – Small, Frequent Meals: Rather than larger meals, eat smaller, more frequent meals to make digestion easier.
- – Monitor Your Body’s Response: Pay attention to how your body responds to different foods. If certain foods cause discomfort, discuss this with your healthcare provider.
Long-Term Diet Maintenance
– Balanced Diet: Maintain a balanced, high-fiber diet long-term for digestive health and to help prevent future flare-ups of diverticulitis.
– Probiotics: Some doctors may recommend probiotics to help maintain a healthy gut environment. Discuss this with your doctor to see if it’s right for you.
Remember, these are general guidelines. Your surgeon or a registered dietitian can give you a personalized eating plan to follow after surgery. It’s important to adhere strictly to the dietary instructions provided by your healthcare professionals to ensure the best possible recovery and long-term health outcomes.